Wellness for Cancer Initiative
2024 Trends
![]()
TREND 1: With Wellness Centers Focused on Longevity, the Impact of Cancer and Its Treatments Need to be a Consideration
TREND 2: Wellness Centers Focus on Longevity: Some Are Considering Early Cancer Detection Tests
TREND 3: Cancer Health & Wellness Coaching Are Growing in Cancer Care
TREND 4: National Cancer Institute (NCI) Continues to Fund Exercise and Nutrition Interventions to Improve Cancer Treatment-Related Outcomes
TREND 5: Studies Examine Feasibility and Clinical Utility of Utilizing Handheld Devices to Detect Breast Cancer
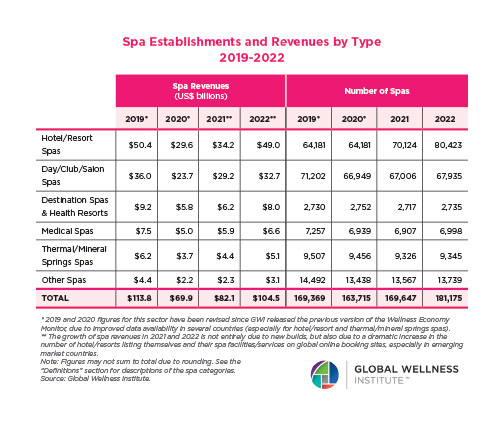
2023 Trends
![]()
TREND 1: Your Lifestyle Matters
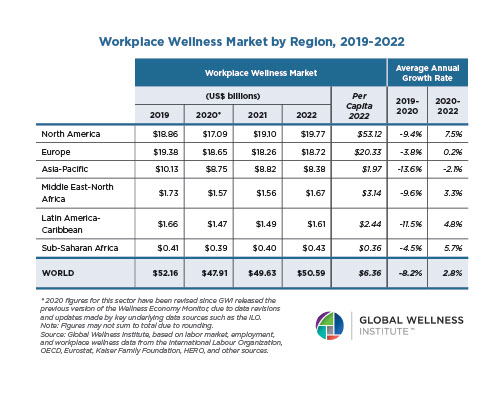
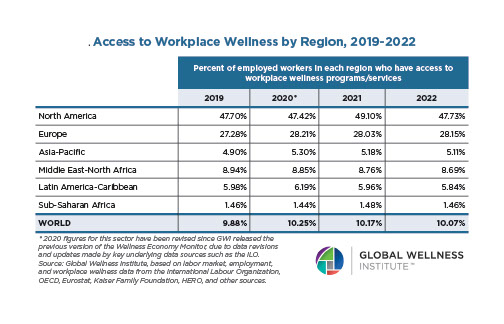
TREND 2: Working with Cancer Comes to the Forefront
TREND 3: Making Integrative Medicine for Cancer Prevention and Cancer Patient Management Understood and Utilized
TREND 4: Gaining a Clearer Understanding of the Global Cancer Burden to Better Address Prevention and Treatment Needs
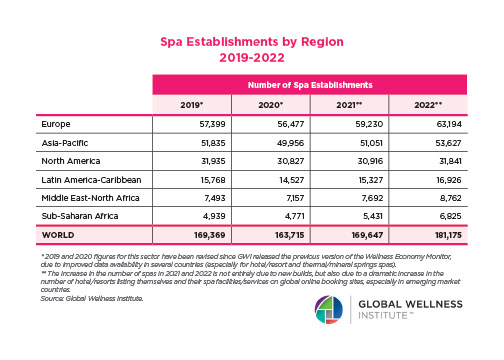
2022 Trends
![]()
Up to 80% of postmenopausal breast cancers are associated with increased estrogen levels.
TREND 1: Dietary options can lower postmenopausal breast cancer risk up to 40%
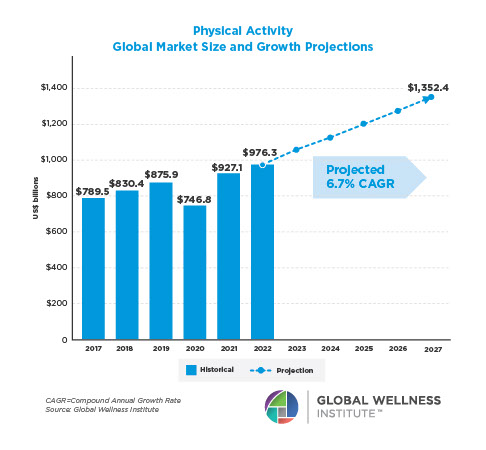
TREND 2: Physical Activity is trending…It’s not too late to influence BC risks
2021 Trends
![]()
TREND 1: The most exciting innovation in early detection–The Galleri test has arrived!
TREND 2: Wellness brands evolve to become more inclusive without ostracizing, stereotyping, or collectively grouping individuals by offering the “cancer” service.
TREND 3: Access to living well and healing evidence and practices from leading doctors and wellness practitioners has never been so readily available.
TREND 4: Yoga and oncology continue to be a priority in clinical research.
TREND 5: Unleashing the power of the immune system as a smart way to prevent, control and eliminate cancer continues to make strides.
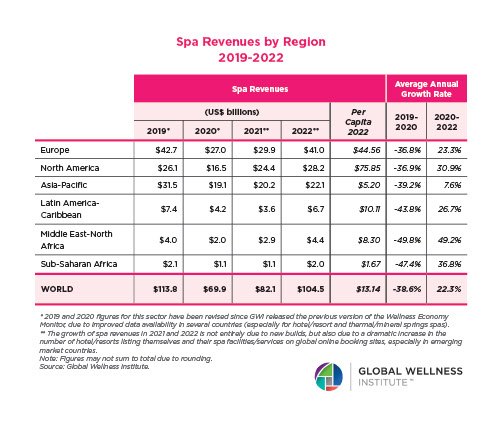
2019 Trends
![]()
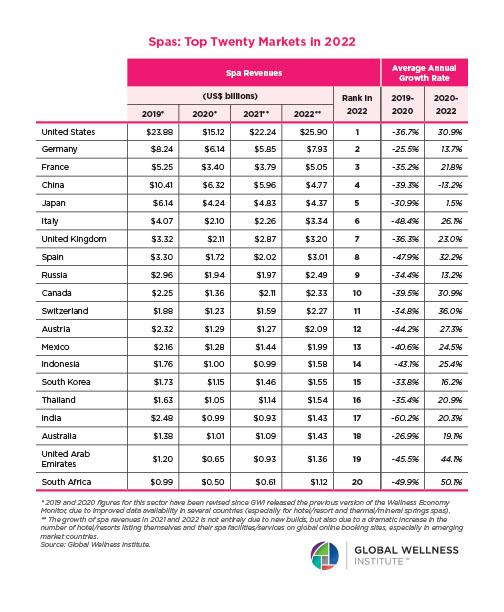
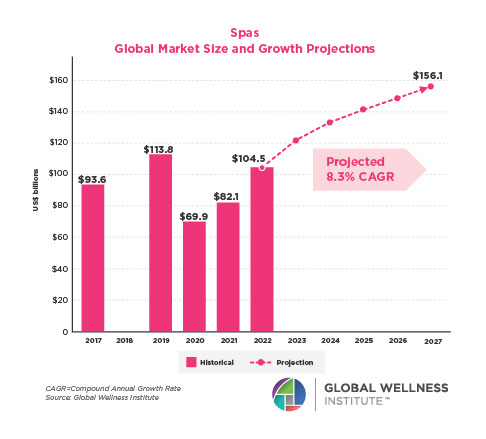
TREND 1: Spa and Wellness Industry becomes serious about being Cancer Aware by establishing minimum education standards
TREND 2: Beauty not only moves to being clean but also into being Cancer Aware
TREND 3: Wellness Brands apply principles of healthy living to people touched by cancer
TREND 4: Sleep programs will address circadian rhythms from cancer prevention through cancer treatment and into survivorship
TREND 5: Menopause programs assist women with lifestyle changes for cancer prevention, through cancer treatment and to prevent the risk of recurrence