Mental Wellness Initiative Resources

Article Series
Interviews

Mental Health Month

Mental Wellness Evidence
Mental Wellness Initiative at the Global Wellness Summit

Mental Wellness Initiative Trends for 2024

Mental Wellness Initiative Trends for 2025

Theme Areas/Working Groups
Video Series
Mental Wellness: Pathways, Evidence and Horizons – Initiative whitepaper
The world is suffering from a mental wellness crisis: Roughly one billion people suffer from anxiety, and one in four people experience mental disorders. This new report from the Global Wellness Institute’s Mental Wellness Initiative answers this need for more evidence-based pathways to mental wellbeing.
DOWNLOAD PAPER

Mental Wellness – The Global Wellness Economy: Looking Beyond COVID
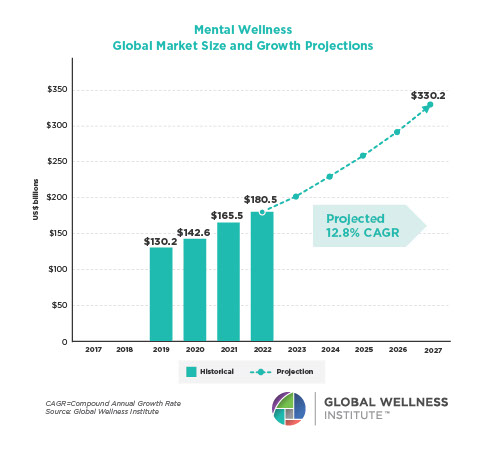
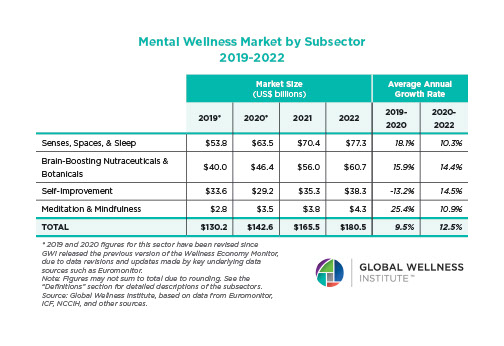
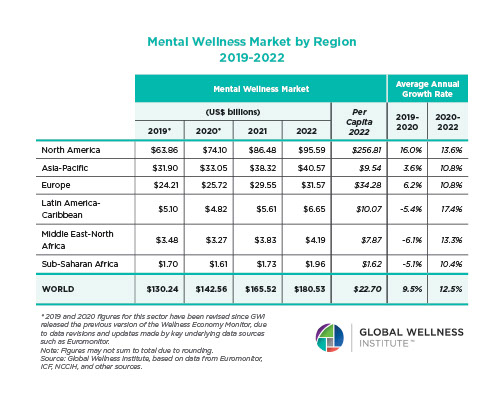
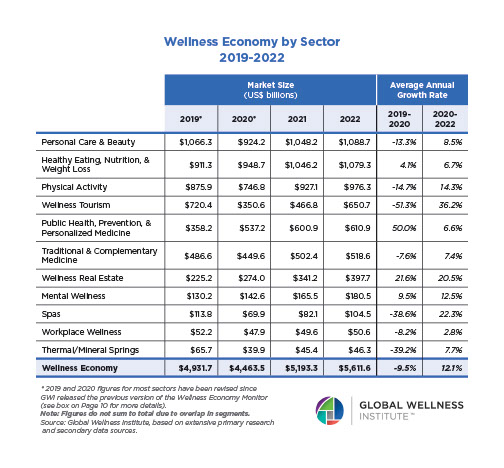
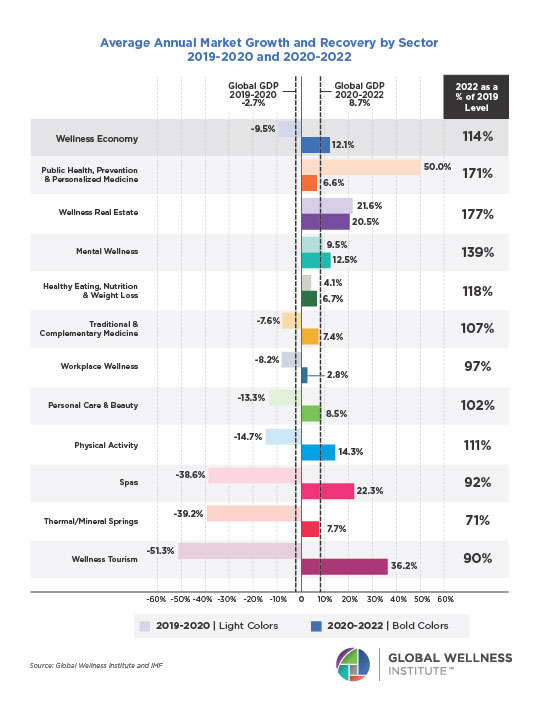
Posted strong 7% growth from 2019-2020 (from a $122 billion to a $131 billion market), as consumers desperately sought solutions to help them cope with pandemic stresses. The largest segment, “senses, spaces and sleep,” grew 12.4%, while the smallest segment, meditation and mindfulness, grew the fastest (25%). The forecast: strong 10% growth annually through 2025, to reach $210 billion.
DOWNLOAD REPORT
The Global Wellness Institute serves as an umbrella organization for numerous Initiatives, that are independently chaired and run. The resources, editorial, research and opinions presented by the Initiatives do not necessarily reflect the opinions of the Global Wellness Institute.