The Future of Brain Health: Lifestyle Medicine, Vascular Vitality, and Neuroplasticity for Lifelong Clarity
How Lifestyle Medicine Pillars, Cardiovascular Health, and Neuroplasticity Create Pathways to Cognitive Preservation Across the Lifespan
Lifestyle Medicine Initiative | January 2026
FOREWORD
Brain health represents the foundation of longevity and healthspan, the years we live with functional independence and vitality. This white paper synthesizes the Lifestyle Medicine Initiative’s webinar “The Future of Brain Health: Lifestyle Medicine, Vascular Vitality, and Neuroplasticity for Lifelong Clarity” into an evidence-informed framework for preserving cognitive function across the lifespan.
It argues that brain health is not an inevitable trajectory toward decline, but a modifiable outcome shaped by lifestyle medicine pillars, vascular risk management, and the brain’s inherent capacity for neuroplasticity. The framework positions brain health as the rate-limiting determinant of exceptional aging living longer with high cognitive and physical function and outlines how nutrition, movement, sleep, stress management, avoidance of risky substances, social connection, and time in nature interact with vascular and neural pathways that govern cognition and mood.
For wellness operators, clinicians, employers, and health systems, this white paper offers a practical blueprint for targeted screening, brain-protective program design, and messaging standards that empower individuals to act on modifiable risk factors.
THE CONTRIBUTORS
Editor: Randi Gold Co Chair Lifestyle Medicine Initiative at the Global Wellness Institute Contributing Authors: Initiative Chair: Melissa Sundermann, DO, DipABLM FACLM; ; Professor Dr Robert Kelly MD MBA FRCPI FACC FESC FFSEM; Alison Levitt, MD
The panel of recognized thought leaders translated cutting‑edge neuroscience and lifestyle medicine evidence into actionable frameworks from three perspectives: the lifestyle medicine foundation, vascular brain health and cardiometabolic risk reduction, and the role of neuroplasticity in adaptive aging and cognitive resilience
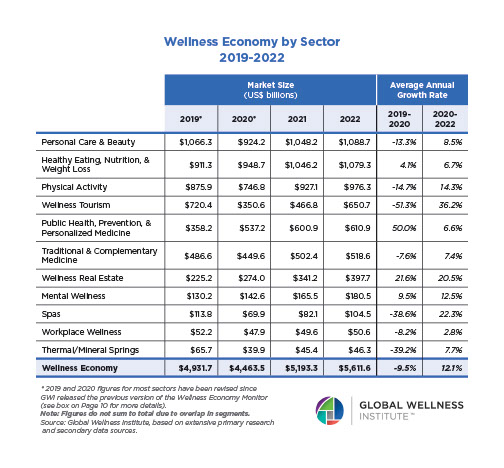
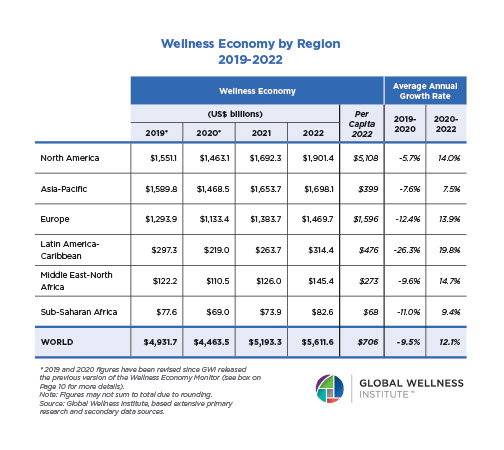
ABOUT THE GLOBAL WELLNESS INSTITUTE
The Global Wellness Institute (GWI), a 501(c)(3) non-profit organization, is considered the leading global research and educational resource for the global wellness industry and is known for introducing major industry initiatives and regional events that bring together leaders and visionaries to chart the future. GWI positively impacts global health and wellness by advocating for both public institutions and businesses that are working to help prevent disease, reduce stress, and enhance overall quality of life. Its mission is to empower wellness worldwide.
ABOUT GWI INITIATIVES
The Global Wellness Institute’s Initiatives support a wide range of industry efforts that advance the growth of multiple sectors within the wellness economy. Led by Initiative Chairs who are renowned thought leaders in their fields, GWI Initiatives have been instrumental in powering the growth of the multi-trillion-dollar wellness economy and uniting the health and wellness industries.
ABOUT THE LIFESTYLE MEDICINE INITIATIVE
The Lifestyle Medicine Initiative at the Global Wellness Institute advances lifestyle medicine as a primary tool for disease prevention, health optimization, and longevity across the wellness and healthcare sectors. We bring together clinicians, researchers, wellness operators, employers, and educators to translate evidence-based lifestyle interventions into scalable, accessible programs that improve health outcomes, reduce chronic disease burden, and extend both lifespan and healthspan.
Our Mission: To educate GWI delegates and the world about the importance of lifestyle and behaviors for health, longevity, mental health, and overall well-being. We bring the best minds in Lifestyle Medicine, the ancient lessons of the world’s healthiest, longest-lived cultures, and principles of positive lifestyle habits—combining lifestyle medicine with evidence-based well-being therapies and 21st-century longevity research to sustainably improve well-being.
Our Goal: To foster sustainable services around wellness and lifestyle medicine that enhance and extend life, and to find the pressure points where healthcare and self-care intersect. Evidence-based lifestyle medicine has emerged as the future of healthcare, controlling costs and delivering better health outcomes by treating root causes of disease. We exchange ideas, build bridges with other GWI Initiatives, and leverage the intersections of well-being innovations to advance longevity through holistic wellness practices.
-
THE FUTURE OF BRAIN HEALTH: LIFESTYLE MEDICINE, VASCULAR VITALITY, AND NEUROPLASTICITY
Brain health is increasingly recognized as the rate-limiting organ of longevity. While aging is inevitable, cognitive decline is not. Emerging evidence from neuroscience, cardiovascular medicine, and lifestyle intervention studies demonstrates that a large proportion of dementia risk—and nearly all preventable cognitive decline—is driven by modifiable lifestyle and vascular factors that can be addressed decades before symptoms arise.
This shift represents a fundamental change in how we approach brain health: from late-stage diagnosis and pharmacologic management to upstream prevention and optimization of protective lifestyle factors. For the global wellness economy—encompassing fitness centers, nutrition coaching, destination wellness, mental health programming, and corporate wellness—this creates both opportunity and responsibility to integrate brain health screening, education, and intervention into their core offerings.
The webinar featured three complementary perspectives:
- Lifestyle Medicine Pillars for Brain Protection (Dr. Melissa Sundermann): How the foundational practices of lifestyle medicine—nutrition, movement, sleep, stress management, substance avoidance, and social connection—directly protect brain structure and function.
- Vascular Vitality as a Brain Health Driver (Dr. Robert Kelly): How cardiovascular health, blood pressure control, management of diabetes and dyslipidemia, and screening for rhythm disorders are essential pillars of cognitive preservation.
- Neuroplasticity and Adaptive Aging (Dr. Alison Levitt): How the brain’s inherent ability to adapt, rewire, and recover function at any age can be leveraged through intentional lifestyle choices and mindset.
Together, these perspectives create a unified, actionable framework for extending both lifespan and healthspan.
II. LIFESTYLE MEDICINE PILLARS AND BRAIN HEALTH
Lifestyle medicine is defined by the American College of Lifestyle Medicine (ACLM) as a medical specialty focused on using evidence-based behavioral interventions—primarily nutrition, physical activity, stress management, adequate sleep, avoidance of risky substances, and positive social connection—to prevent, treat, and reverse chronic disease.
For brain health specifically, each pillar plays a distinct yet interconnected role:
A. Nutrition and the MIND/Mediterranean Dietary Pattern
The MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) combines evidence from Mediterranean and DASH (Dietary Approaches to Stop Hypertension) patterns to emphasize foods most strongly associated with cognitive preservation.
Key components:
- Abundant vegetables, fruits, whole grains, legumes, nuts, and seeds
- Moderate fish and low-fat dairy
- Minimal red meat, processed foods, added sugars, and saturated fats
- Plant-forward orientation
Evidence: Multiple large cohort studies and randomized controlled trials demonstrate that adherence to plant-rich dietary patterns is associated with:
- Reduced dementia incidence and delayed cognitive decline
- Better preserved gray matter volume and white matter integrity
- Lower amyloid and tau biomarker accumulation (measured in blood and cerebrospinal fluid)
- Reduced inflammatory markers (IL-6, TNF-α, CRP)
Implementation: Wellness centers can offer plant-forward cooking classes, nutrition consultations focused on the MIND/Mediterranean pattern, and community education on anti-inflammatory foods.
B. Movement and BDNF: “Miracle-Gro for the Brain”
Physical activity is one of the most robust protective factors against cognitive decline and dementia risk. The mechanism is partly understood through increased production of brain-derived neurotrophic factor (BDNF), a growth protein that supports neuronal survival, growth, and synaptic plasticity.
Evidence:
- Higher daily step counts associated with lower dementia risk and better cognitive function
- Aerobic exercise increases hippocampal volume and improves memory
- Resistance training enhances executive function and processing speed
- Regular movement is protective even in the presence of Alzheimer’s pathology
Implementation: Fitness centers, personal training, group classes, and workplace movement programs can emphasize brain-protective benefits of regular physical activity, not solely weight loss or appearance.
C. Sleep and the Glymphatic System
Sleep is when the brain’s “glymphatic system”—a waste clearance mechanism—is most active. During sleep, cerebrospinal fluid flushes accumulated metabolic byproducts, including amyloid-beta and tau proteins, from the brain. Sub-optimal sleep is associated with increased dementia risk.
Evidence:
- Chronic sleep deprivation (< 6 hours/night) linked to 30% increased dementia risk
- Sleep apnea (a common, often undiagnosed condition) is an independent risk factor for cognitive decline
- Sleep disruption impairs memory consolidation and emotional regulation
- Midlife sleep loss (age 50–65) has particularly strong dementia associations
Implementation: Wellness centers can offer sleep hygiene education, circadian rhythm workshops, referral pathways for sleep apnea evaluation, and relaxation/meditation programs that improve sleep quality.
D. Stress Management, Substance Avoidance, Social Connection, and Nature Exposure
Chronic stress elevates cortisol and inflammatory markers, both linked to neurodegeneration. Social isolation is comparable to smoking 15 cigarettes per day as a dementia risk factor. Time in nature and stress-reducing practices (meditation, yoga, breathing) are protective.
Evidence:
- HHS Surgeon General report on loneliness identifies social isolation as major health risk
- Mindfulness and meditation increase gray matter density in attention and emotional regulation regions
- Nature exposure reduces stress hormones and supports cognitive function
- Alcohol and tobacco use accelerate cognitive decline
Implementation: Group classes (yoga, tai chi, meditation), guided nature walks, group health coaching, community events, and workplace stress-reduction initiatives all amplify this pillar.
III. VASCULAR VITALITY AS A BRAIN HEALTH DRIVER
The brain depends on a continuous, well-regulated blood supply to function. When cerebral blood vessels become damaged or dysfunctional—due to hypertension, diabetes, chronic inflammation, or atherosclerosis—the result is reduced oxygen delivery, increased inflammation, and accelerated neurodegeneration.
Critically, the same cardiovascular risk factors that lead to heart attack and stroke also drive dementia. A person with hypertension, atrial fibrillation, diabetes, or obesity carries elevated risk for both cardiovascular disease and cognitive decline.
A. The Shared Risk Factor Model
Major modifiable risk factors for vascular brain health include:
- Hypertension (high blood pressure)
- Diabetes and metabolic syndrome
- Dyslipidemia (abnormal cholesterol)
- Obesity
- Sedentary lifestyle
- Sleep apnea
- Atrial fibrillation (irregular heart rhythm)
- Smoking and tobacco use
- Excessive alcohol consumption
B. Stroke, Atrial Fibrillation, and Dementia
Stroke—even subclinical “silent” strokes—is a major driver of cognitive decline. Atrial fibrillation (AFib), a condition affecting 2–3% of the adult population, significantly increases dementia risk through both embolic stroke and chronic cerebral hypoperfusion.
Key insight: A person with undiagnosed or unmanaged AFib may not have experienced a major stroke but may accumulate multiple small cerebral infarcts, leading to gradual cognitive decline years or decades before a diagnosis of dementia is made.
C. The Lancet Life-Course Model
The Lancet Commission on dementia prevention has identified a life-course model of modifiable risk factors, showing that interventions at midlife (ages 40–65) have outsized protective impact on late-life cognition. Vascular risk factor management during this window is critical.
D. Clinical and Wellness Implications
Screening:
- Routine blood pressure monitoring and hypertension management
- Fasting glucose or HbA1c (diabetes screening)
- Lipid panel (total cholesterol, LDL, HDL, triglycerides)
- Cardiac rhythm awareness (pulse checks, ECG for AFib risk)
- Sleep apnea screening (STOP-BANG questionnaire)
Intervention:
- Weight optimization through nutrition and movement
- Blood pressure reduction via lifestyle and, if needed, medication
- Diabetes prevention/management through diet and exercise
- Lipid management
- AFib identification and anticoagulation if indicated
-
NEUROPLASTICITY AND ADAPTIVE AGING
Neuroplasticity—the brain’s ability to adapt, rewire, and recover function in response to internal and external inputs—was once believed to decline sharply after childhood. We now know this is false. The adult brain retains remarkable capacity for structural and functional change throughout life.
A. What is Neuroplasticity?
Neuroplasticity includes:
- Structural plasticity: The brain can reorganize, form new neural connections (synapses), and even generate new neurons (neurogenesis) in the hippocampus (memory center) and prefrontal cortex (executive function).
- Functional plasticity: If one brain region is damaged, other regions can compensate and take over functions.
- Long-term potentiation and depression: The strengthening or weakening of synaptic connections based on use—the basis of learning and memory.
B. Lifestyle Inputs That Drive Plasticity
Nutrition: Provides building blocks (amino acids, omega-3 fatty acids, vitamins, minerals) for synaptic repair and myelin formation.
Movement and aerobic exercise: Increases BDNF, supports hippocampal neurogenesis, and enhances executive function.
Learning and cognitive challenge: Engages prefrontal cortex, builds synaptic density, and delays cognitive aging.
Sleep: Consolidates memories and supports synaptic pruning and waste clearance.
Stress reduction and relaxation: Lowers cortisol and supports parasympathetic nervous system tone, creating conditions for neural repair.
Social engagement: Activates multiple brain regions, challenges executive function, and builds cognitive reserve.
C. Hope for Midlife and Beyond
Neuroplasticity offers profound hope to individuals already experiencing brain fog, mild cognitive impairment, or menopause-related cognitive changes. With intentional lifestyle inputs and mindset shifts, the brain can improve, recover, and build resilience even after years of suboptimal habits.
V. RECOMMENDATIONS FOR WELLNESS, HEALTHCARE, AND EMPLOYER IMPLEMENTATION
A. For Wellness Centers and Destinations
- Brain Health as a Core Program: Develop integrated brain-health retreats and programs that combine movement, nutrition, stress management, sleep optimization, and social connection.
- Staff Education: Train fitness professionals, nutritionists, and wellness coaches in brain health science so they can speak competently about cognitive protection and neuroplasticity.
- Brain-Specific Fitness Programming: Emphasize movement classes that challenge balance, coordination, and cognitive function (e.g., dance, martial arts, group fitness with cognitive tasks), not just cardiovascular benefits.
- Nutrition Programs: Offer MIND/Mediterranean-inspired cooking classes, plant-forward meal planning, and nutrition education with brain health framing.
- Sleep and Stress Workshops: Host sleep hygiene seminars, meditation/mindfulness classes, and relaxation programming.
- Measurement and Outcomes: Use simple screening tools (e.g., Montreal Cognitive Assessment, self-report cognitive function) and track lifestyle adherence to demonstrate early impact.
- Referral Pathways: Develop relationships with local clinicians for participants who may need medical evaluation (e.g., sleep apnea, hypertension, AFib screening).
B. For Healthcare Systems and Clinicians
- Integrated Screening: Use cognitive function, vascular risk, and lifestyle assessments as routine components of preventive care, especially at midlife (age 40+).
- Referral to Wellness Programming: Direct patients to lifestyle-focused wellness centers, group medical visits, and community programs rather than relying solely on pharmacotherapy.
- Interdisciplinary Teams: Collaborate with lifestyle medicine practitioners, nutritionists, fitness professionals, and mental health providers to create comprehensive brain-health programs.
- Patient Education: Empower patients with evidence that cognitive decline is preventable and that lifestyle choices directly impact brain health.
C. For Employers and Corporate Wellness
- Brain Health Initiatives: Develop workplace brain-health programs including movement breaks, nutritious food options, stress management workshops, and cognitive challenges.
- Cardiometabolic Risk Reduction: Integrate blood pressure monitoring, glucose screening, and weight management with brain-health messaging.
- Sleep and Stress: Provide sleep education, meditation apps, and mental health support.
- Community and Connection: Foster workplace social connection, team activities, and community service -all protective for brain health.
- Messaging: Reframe wellness initiatives with brain health as the priority: “Invest in your brain today; enjoy cognitive clarity and independence throughout your life.”
SOURCES: ACCESS THE RECORDING
Lifestyle Medicine Initiative at the Global Wellness Institute. The Future of Brain Health: Lifestyle Medicine, Vascular Vitality, and Neuroplasticity for Lifelong Clarity (webinar recording, February 2025).
American College of Lifestyle Medicine. What is Lifestyle Medicine?
Alzheimer's Association. The MIND Diet.
HHS Office of the Surgeon General. Our Epidemic of Loneliness and Isolation.
The Lancet Commission on Dementia Prevention, Intervention, and Care.
American Stroke Association. Stroke Prevention and Warning Signs.
xxxxxxxx