How Culinary Medicine and Teaching Kitchens Translate Nutrition Science into Sustained Behavior Change and Disease Prevention
Culinary Medicine and Teaching Kitchens Translate Nutrition Science into Sustained Behavior Change and Disease Prevention
Lifestyle Medicine Initiative | January 2026 | Webinar RecapCulinary medicine and teaching kitchens translate nutrition science into sustained behavior change by “blending nutrition education and culinary skill building” so “nutrition [is] doable in real life,” not just understood in theory.
The approach is explicitly designed to be “Approachable,” “Skill-Based,” “Culturally Familiar,” and “Budget Friendly,” and the deck emphasizes that durable results require more than information alone because “Education is Necessary but Not Sufficient” and “Behavior change is rooted in science,” requiring preparation, “the right strategy at the right time,” and “small changes” that can lead to “big results is the most powerful medicine most people have access to every day. Practically, the deck illustrates culinary medicine as an “evidence-based field” that brings “nutrition knowledge and the art of cooking” together and can “show up in healthcare, employee health and your own kitchen, supporting wellness operators, health systems, employers, clinicians, and individuals seeking practical healthy solutions and guidance through food. Our panel gave evidence based food-as-medicine programming examples that aligns with clinical evidence and GWI’s standards for integrity and responsible communications.
Moderator Randi Gold, Co-Chair,Lifestyle Medicine Initiative at The Global Wellness Institute
Expert Panel | Contributors Initiative Chair Melissa Sundermann, DO, DipABLM FACLM;Debora Duro MD, MS Pediatric GI, Nutrition Support, Culinary Medicine; Dr. Leanne Mauriello, PhD
ABOUT THE GLOBAL WELLNESS INSTITUTE
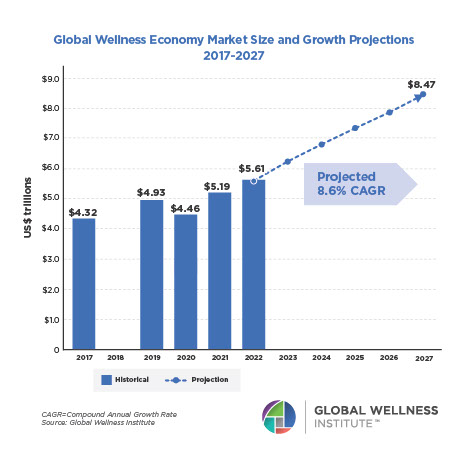
The Global Wellness Institute (GWI), a nonprofit 501(c)(3), is considered the leading global research and educational resource for the global wellness industry and is known for introducing major industry initiatives and regional events that bring together leaders to chart the future. GWI positively impacts global health and wellness by educating public institutions, businesses and individuals on how they can work to prevent disease, reduce stress and enhance overall quality of life. Its mission is to empower wellness worldwide.
ABOUT GWI INITIATIVES
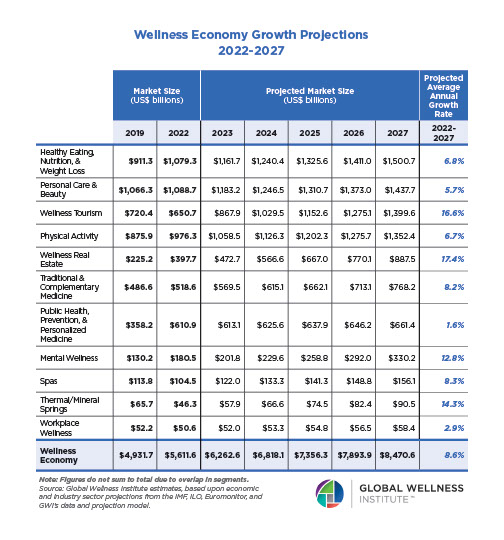
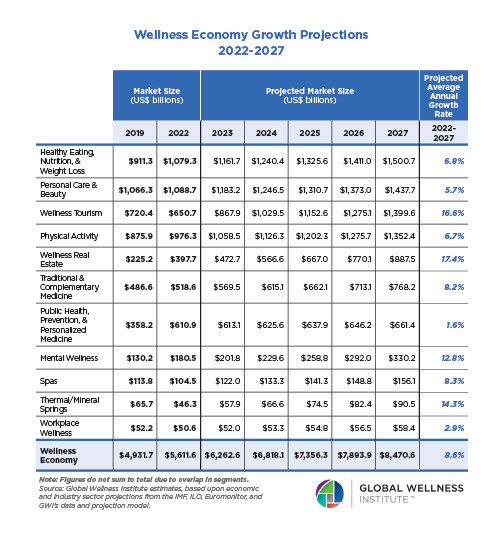
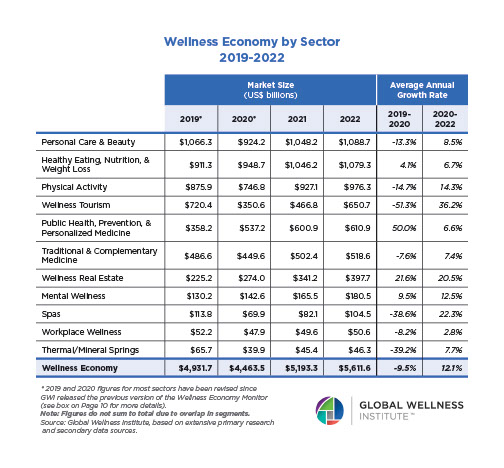
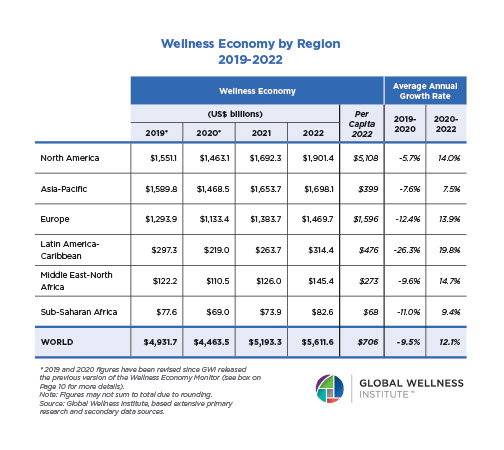
The Global Wellness Institute’s Initiatives support a wide range of industry efforts that advance the growth of multiple sectors within the wellness economy. Led by Initiative Chairs who are renowned thought leaders in their fields, GWI Initiatives have been instrumental in powering the growth of the multi-trillion-dollar wellness economy and uniting the health and wellness industries.
ABOUT THE LIFESTYLE MEDICINE INITIATIVE
The Lifestyle Medicine Initiative at the Global Wellness Institute advances lifestyle medicine as a primary tool for disease prevention, health optimization, and longevity across the wellness and healthcare sectors. We bring together clinicians, researchers, wellness operators, employers, and educators to translate evidence-based lifestyle interventions into scalable, accessible programs that improve health outcomes, reduce chronic disease burden, and extend both lifespan and health span with lifestyle medicine as the foundation.
Our Mission: To educate GWI delegates and the world about the importance of lifestyle and behaviors for health, longevity, mental health, and overall well-being. We bring the best minds in Lifestyle Medicine, the ancient lessons of the world’s healthiest, longest-lived cultures, and principles of positive lifestyle habits combining lifestyle medicine with evidence-based well-being therapies and 21st-century longevity research to sustainably improve well-being.
Our Goal: To foster sustainable services around wellness and lifestyle medicine that enhance and extend life, and to find the pressure points where healthcare and self-care intersect. Evidence-based lifestyle medicine has emerged as the future of healthcare, controlling costs and delivering better health outcomes by treating root causes of disease. We exchange ideas, build bridges with other GWI Initiatives, and leverage the intersections of well-being innovations to advance longevity through holistic wellness practices.
Food as medicine became real when healthcare professionals literally moved into the kitchen and this Global Wellness Institute webinar showed how that shift could prevent treat and even help reverse chronic disease By blending lifestyle medicine nutrition science and culinary medicine the expert panel demonstrated that everyday meals were one of the most powerful tools available to improve health and extend health span
The conversation explored three key questions. Why did unhealthy food drive inflammation and disease? What did food as medicine look like in daily life? How could behavior change science help people reclaim their health one meal at a time? This directly supported the Global Wellness Institute mission to empower wellness worldwide by turning cutting edge research into practical strategies that could be used by individuals workplaces and communities
Dr. Melissa Sundermann, DO, FACOI, DipABLM, FACLM, an endurance athlete, founder of Doctor Outdoors, and Co-Chair of the Global Wellness Institute’s Lifestyle Medicine Initiative opened by defining lifestyle medicine. She explained that it is the use of a whole-food, plant-predominant dietary pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection as primary therapeutic tools for the treatment and potential reversal of chronic disease.
She described these six pillars as simple powerful therapy when they were applied consistently. Over time Sundermann reminded viewers that conditions such as type 2 diabetes hypertension high cholesterol and even advanced coronary artery disease were not only preventable but actually reversible when comprehensive lifestyle changes were implemented under medical guidance.
For Dr. Sundermann , food was foundational. She stated that food was medicine and explained that lifestyle medicine advocated a plant forward plant strong dietary pattern . She defined a whole food plant based diet as a dietary pattern centered on minimally processed vegetables fruits whole grains and legumes with nuts and seeds in moderation while minimizing or excluding meat dairy eggs added sugars and processed oils.
On a practical level she encouraged people to eat the rainbow by filling half the plate with colorful fruits and vegetables. One quarter with whole grains, such as brown rice or quinoa and one quarter with plant proteins such as beans, lentils tofu, and a variety of nuts and seeds. Quoting Michael Greger MD she highlighted the goal of choosing foods where nothing bad was added and nothing good was taken away , and she echoed Michael Pollan by saying, “Eat food, Not too much Mostly plants.”
Dr. Sundermann shared evidence based benefits of this way of eating, including lower body mass index and body fat which reduced overall mortality. Lower mortality from ischemic heart disease , as well as reduced need for medications. She noted that plant based patterns were associated with reduced incidence of hypertension hyperlipidemia and hyperglycemia reduced risk of certain cancers, especially colorectal cancer and even reversal of advanced coronary artery disease and type 2 diabetes in landmark studies.
She emphasized that a plant based diet supported living longer and more importantly supported living longer in good health. In her words, “The real goal was not only to extend lifespan but to extend health span and well span so that people could remain active engaged and vibrant as they aged.”
Dr. Deborah Duro, MD MS gastroenterologist and Medical Director of the Intestinal Rehabilitation Program at Nicklaus Children’s Health System, with advanced training in culinary coaching from Harvard Medical School and expertise in pediatric nutrition support and culinary medicine defined food as medicine as the result of integrating food into the management prevention, and in some cases even reversal of diseases. She explained that the food people ate could interact with metabolic pathways through pharmacologic properties either directly or indirectly and in this way regulated biochemical cellular processes throughout the body.
Dr. Duro pointed to headlines that said their food was killing too many of them and noted that diet had become the number one predictor of all cause mortality surpassing tobacco in recent years. She highlighted data showing that fewer than ten percent of people in the United States met recommended dietary goals and that this chronic underconsumption of fruits vegetables and fiber created a stage for a weak immune system and widespread non communicable disease.
She described the Standard American Diet as a diet in crisis This pattern was high in ultra processed foods animal products excess calories saturated fats sodium refined carbohydrates and added sugars and low in fruits vegetables nuts seeds and fiber which collectively promoted chronic disease and weakened immune function
Dr. Duro explained how ultra processed foods with their emulsifiers colorants sweeteners and refined oils damaged the tight junctions of the intestinal lining, increased permeability and contributed to dysbiosis an unhealthy imbalance in the gut microbiome. This set off a cascade of systemic inflammation that increased the risk of a range of conditions from cardiovascular disease to metabolic syndrome and autoimmune disorders.
She then presented an anti inflammatory way of eating as both prevention and therapy. An anti inflammatory diet she explained, was rich in vegetables of many colors relied on plant sources of protein such as legumes soy nuts and seeds included whole grains as the primary source of carbohydrates and used healthy fats that were rich in monounsaturated fatty acids and omega 3 fatty acids along with herbs and spices that added antioxidants and flavor.
Dr. Duro highlighted five key mechanisms through which this anti inflammatory plant forward pattern promoted health and longevity . These included a lipid lowering effect from reduced saturated fat , increased healthy fats protection against oxidative stress and inflammation, modulation of hormones and growth factors involved in the pathogenesis of cancer, reduced methionine intake which had been associated with longer lifespan, and protection against chronic disease and improvement of gut microbiota diversity and production of short chain fatty acids.
She then turned to concrete food as medicine strategies that were already in use in healthcare settings . These included medically tailored meals and groceries , therapeutic diets and personalized meal plans , produce prescriptions and community programs that expanded access to healthy foods , as well as culinary medicine programs that helped people learn how to shop cook and eat in alignment with their health goals.
Incorporating food into treatment plans she noted , could decrease the number of medications needed and reduce overall healthcare costs while improving control of chronic conditions and reducing hospital admissions. She defined culinary medicine as an evidence based field that brought together nutrition and culinary knowledge to assist patients in maintaining health and in preventing and treating disease by choosing high quality healthy foods together with appropriate medical care.
Dr. Leanne Mauriello, PhD a behavior scientist and lifestyle medicine pioneer, and Executive Director of the Bonnie Wesorick Center for Healthcare Transformation then focused on how the team had turned knowledge into action through culinary medicine. Her work sat at the intersection of behavior change science and culinary and lifestyle medicine and she shared that in decades of designing health programs she had rarely seen anything as effective as well designed culinary medicine in helping people make meaningful changes to their dietary behaviors.
She explained that culinary medicine was not about gourmet restaurant style cooking or complex recipes. Instead it was about making recipes food and cooking approachable and budget friendly and ensuring that meals were culturally familiar, health promoting and skill based so that people felt confident cooking at home with the time money and tools they actually had..
Mauriello traced the growth of the field including the launch of the Goldring Center for Culinary Medicine at Tulane University School of Medicine in 2012 , the first medical school to have a chef on faculty and a dedicated teaching kitchen. She noted that by 2023 culinary medicine had become visible enough to earn a cover story in Today s Dietitian, a sign that this approach was increasingly recognized within nutrition and medical education.
She described Lifestyle Medicine HQ , a teaching kitchen hub where culinary medicine classes were brought to life for clinicians patients and community members . Photos from the program showed participants cooking tasting and learning together, and Mauriello noted that there were many smiles laughter and aha moments as people discovered how delicious healthy food could be.
She shared outcomes from a Cooking for Health shared medical appointment series designed for individuals with obesity and or chronic disease that used a Food as Medicine intervention over six months. Delivered by a physician and chef, as a series of five shared medical appointments with group medical nutrition therapy this program achieved measurable improvements in body mass index A1C and cholesterol among seventy seven participants.
Drawing on her behavior change background Dr. Mauriello emphasized that education was necessary but not sufficient. People needed more than information. They needed skills, inspiration and community to translate knowledge into lasting habits and that was where culinary medicine teaching kitchens and group programs could be transformative.
She outlined principles of behavior change science noting that behavior change was rooted in science not luck or willpower alone. Evidence based strategies could support lasting change but only when the right strategies were used at the right time, and when people shifted from thinking about change to preparing for it. Taking action and sustaining small steps over time.
Dr. Mauriello explained that change required patience and realistic expectations. Attempts often failed when people took on too big a change at once tried to change many things at the same time , jumped in without preparation or expected immediate perfect results . She encouraged viewers to see change as a journey and to meet patients and people where they were instead of expecting them to leap to an ideal lifestyle overnight.
She offered a different perspective in which big change happened one step at a time through small sustainable actions. Examples included drinking more water, adding an extra serving of vegetables each day , or swapping refined grains for whole grains. These small shifts could add up to significant health gains especially when they were reinforced by supportive programs and communities.
One example she highlighted was a fifteen day Whole Food Plant Based Jumpstart Program also called a Palate Reset that gave people a short intensive experience of eating in a new way. Participants often saw improvements in cholesterol blood pressure and other metrics in just over two weeks while also retraining their taste buds to enjoy less processed more natural flavors.
Throughout the webinar moderator Randi Gold brought the ideas together into practical takeaways viewers could apply immediately. Click Here for the “Bringing Healthcare Into The Kitchen, Harnessing the Power of Food as Medicine Webinar”
From Dr. Melissa Sundermann, the message was that food was foundational and that a whole food plant predominant lifestyle was one of the most powerful tools available to prevent and even reverse many chronic diseases while extending health span.
From Dr. Debora Duro , the central insight was that every bite of food talked to their cells influencing inflammation hormones, metabolic pathways and the gut microbiome. This meant that shifting away from ultra processed foods toward anti inflammatory high fiber meals could fundamentally change their health trajectory.
From Dr. Leanne Mauriello, PhD, the key was that small doable steps combined with culinary skills inspiration and community support were what made healthy eating stick in real life.
Taken together the voices of Sunderman, Duro, and Mauriello showed that when healthcare moved into the kitchen practitioners and patients did more than treat disease. They built a new model of care in which food as medicine lifestyle medicine and culinary medicine worked together to help people reclaim their health and enjoy delicious nourishing food every day.
Slide deck source link Bringing-Healthcare-Into-The-Kitchen-Harnessing-The-Power-Of-Food-As-Medcne.pdf